Explore All Articles
Explore All Articles

If you only take four ideas from this article, make them these:
If you’re brand new to CoQ10, start with the foundational primer:
What Is Coenzyme Q10? Its Benefits for Health, Energy, and Aging
Your heart is a relentless engine. Even when you’re asleep, it’s contracting - pushing blood through miles of vessels, delivering oxygen and nutrients to every organ that’s quietly doing its own jobs.
That constant work comes with two big biological demands:
Coenzyme Q10 (CoQ10) gets attention in heart health because it sits at the intersection of both demands: it’s involved in mitochondrial energy transfer and participates in redox cycling (the chemical “flip-flop” between oxidized and reduced forms that underlies antioxidant function).
CoQ10 exists in different interconverting forms, and understanding them helps the rest of the story make sense. For those interested, more on the deeper science of these forms can be found at: The Three Faces of CoQ10: Ubiquinone, Ubiquinol, and Semi-Ubiquinone
When supplement claims get confusing, it’s usually because different kinds of evidence are being mixed together like they’re the same thing.
Mechanisms matter. They’re the “why it could work.” But clinical results are the “does it work in your life.”
To keep things honest, we’ll separate:
If you zoom into a heart muscle cell, you’ll see it’s loaded with mitochondria—tiny organelles that function like power plants. Mitochondria turn energy from food (fatty acids and glucose) into ATP (adenosine triphosphate), the energy “currency” that powers the cells activities - including contraction.
CoQ10 lives in the inner mitochondrial membrane and helps shuttle electrons through the electron transport chain - a stepwise process that drives ATP production. 8
If you want a clear, step-by-step walk-through of how CoQ10 supports ATP production across tissues (including muscle and heart), see:
CoQ10 and Cellular Energy: How This Molecule Powers Every Cell in Your Body
Could CoQ10 help your heart make energy more efficiently?
Here’s the relatable question: Have you ever felt like your body has the will to do something, but not enough energy to do it? In certain heart conditions, the issue isn’t motivation - it’s cellular energy handling.
Your heart is an energy hog. It beats around 100,000 times per day, which means its cells need a steady supply of ATP.1, 2 It’s also extraordinarily metabolically active: classic physiology work shows the myocardium’s energy handling is intense and dynamic.2, 9
That doesn’t automatically mean “you need supplements,” but it explains why mitochondria matter in cardiovascular physiology and why CoQ10 is relevant.2
CoQ10 cycles between oxidized and reduced states. The ubiquinone form is often discussed in the context of electron transport, because this redox cycling is how CoQ10 helps move electrons along the chain.5, 8
If you want a heart-specific “mitochondria + CoQ10” explainer written for non-biochemists, see:
Energize Your Heart – The CoQ10 Connection
If energy production is the “power” story, oxidative stress is the “wear-and-tear” story.
A free radical is a reactive molecule with an unpaired electron. That unpaired electron makes it chemically restless - like a person who shows up to a potluck and starts stealing food off other people’s plates.
Free radicals can be useful in controlled amounts (immune defense uses them), but in excess they can attack:
Oxidative stress happens when oxidant production outpaces antioxidant defenses. Over time, that imbalance can contribute to dysfunction in many tissues—including cardiovascular tissues. CoQ10 is relevant because it participates in antioxidant defense and redox cycling, particularly in its ubiquinol form.5
If you want a dedicated explainer you can send to a friend who thinks “oxidative stress” is just marketing jargon, read:
CoQ10: A Powerful Ally Against Oxidative Stress
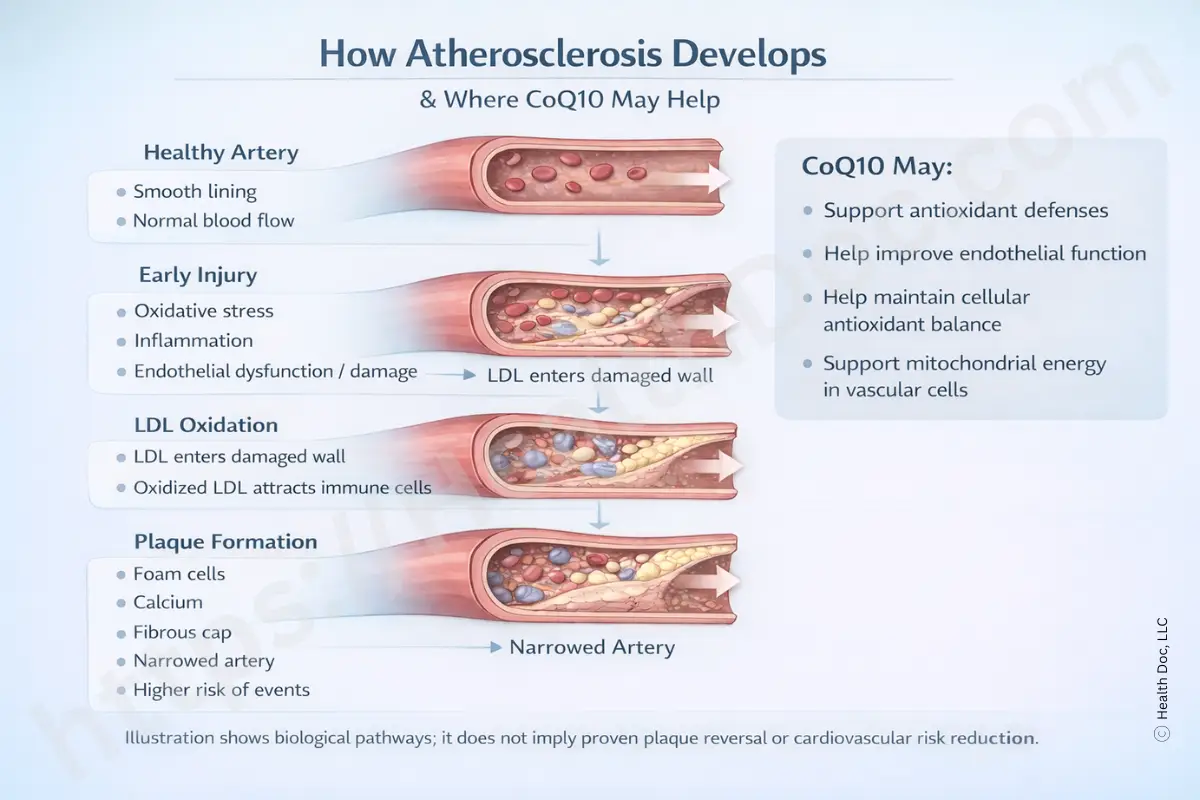
You’ll often see CoQ10 mentioned alongside LDL oxidation because oxidation biology is part of atherosclerosis research conversations. But it’s easy to overclaim here.
In other words: plausible mechanism ≠ guaranteed clinical result. We’ll keep that distinction intact later when we talk about atherosclerosis.
Even a strong heart struggles if the “pipes” aren’t responsive.
The endothelium is the thin layer of cells lining blood vessels. It helps regulate:
Endothelial health is a major theme in cardiovascular disease research.10
Because oxidative stress can disrupt endothelial signaling, and CoQ10 participates in redox biology, it’s biologically plausible that CoQ10 could influence endothelial function in some contexts.5, 10
If blood pressure is your main interest, you can find more here:
CoQ10 and Blood Pressure: Can This Natural Supplement Help?
Here’s the big question: If CoQ10 is so fundamental, why isn’t it a slam dunk for every heart condition?
Because heart disease isn’t one thing. “Heart problems” can involve:
CoQ10 would be expected to matter most when energy handling and oxidative stress are meaningfully part of the bottleneck.
If you’ve ever heard “statins deplete CoQ10,” you’re hearing a simplified version of a real biochemical connection.
Statins inhibit HMG-CoA reductase, which affects the mevalonate pathway - a pathway involved in producing cholesterol and also involved upstream in CoQ10 synthesis. Studies have documented decreases in CoQ10 levels with statin use.6, 7
If statins are part of your story, start here:
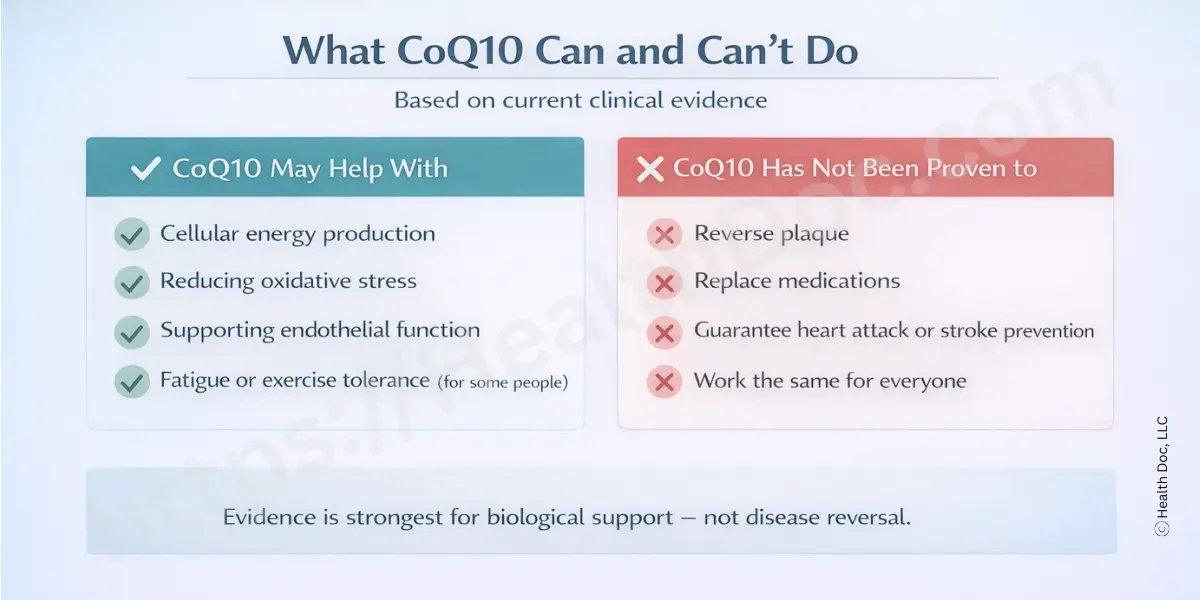
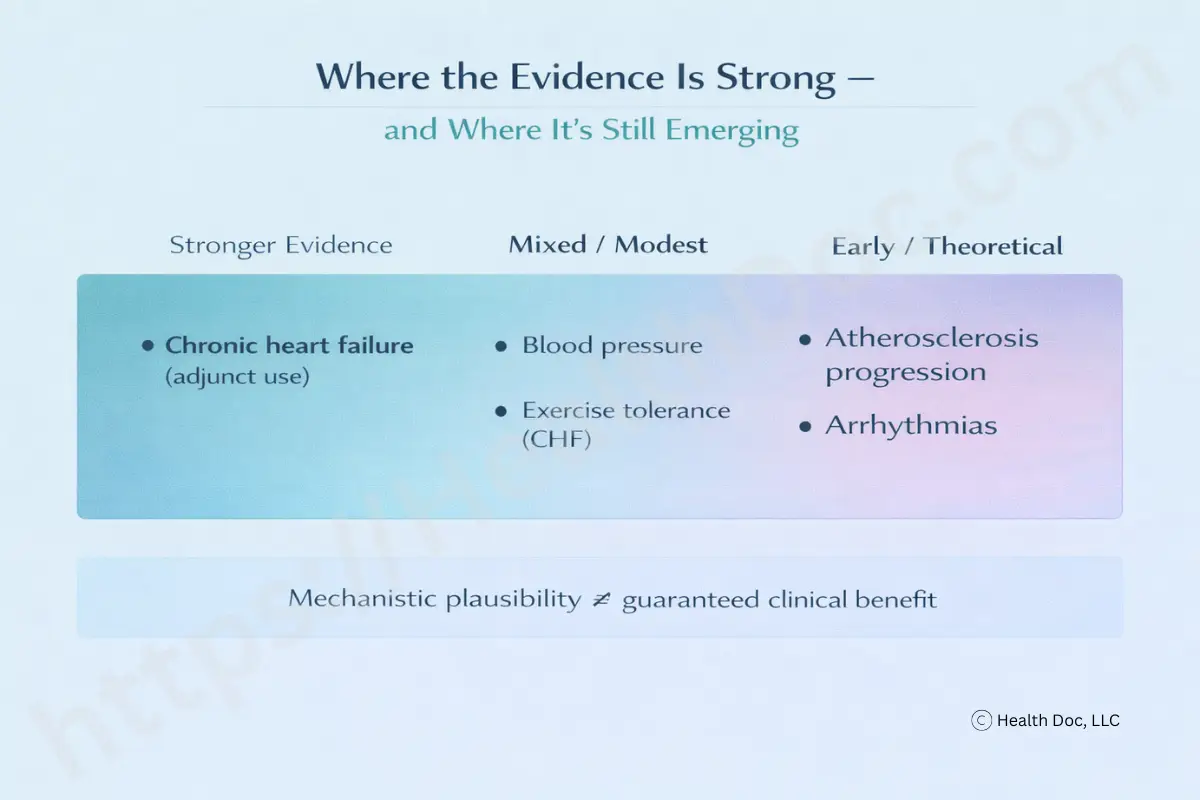
This is where it helps to shift from “Does it work?” to “In whom, for what outcome, and how reliably?”
Within the cited research set:
CoQ10 has been studied as an adjunct in chronic heart failure, and some trials suggest improvements in outcomes such as morbidity and mortality, as well as symptom-related measures, when used alongside standard therapy.3 Meta-analytic work also supports the idea that CoQ10 may be beneficial in CHF contexts.5
A crucial point: adjunct doesn’t mean “replacement.” It means something used alongside guideline-based care.
A meta-analysis suggests CoQ10 can lower blood pressure in some trials.4 That doesn’t mean everyone with hypertension will respond. Blood pressure is influenced by salt sensitivity, vascular tone regulation, kidney function, stress hormones, sleep quality, and medication adherence - so variability is expected.
Some work suggests combining CoQ10 with exercise training may offer benefit in CHF populations, which fits a broader theme: supplements tend to perform best when paired with lifestyle and medical strategy rather than used alone.12
CoQ10 is generally considered well tolerated in studies, including at higher doses.15 But “well tolerated” doesn’t mean “never causes side effects.”
Some people report:
If you’re trying to decide whether low CoQ10 status might even apply to you, this can help frame the question: Signs of CoQ10 Deficiency: What Your Body Might Be Telling You
If you’ve ever wondered why supplement research rarely ends in a simple “yes” or “no,” here’s the honest answer: biology is complicated and studies are messy.
Common limitations include:
These limitations are why it’s fair to feel cautiously optimistic while still demanding better trials.20
Think of heart health as a dashboard, not a single gauge. CoQ10, at best, may improve one set of dials (energy/redox capacity), but your overall cardiovascular risk and outcomes are heavily influenced by:
That’s why heart-health organizations emphasize lifestyle foundations.21 And yes—stress and depression aren’t just “in your head.” They measurably influence cardiovascular risk pathways.22
If you want a practical “systems-level” companion read:
Boost Your CoQ10 Levels Naturally: Best Foods, Lifestyle Tips & Supplements
Here’s a practical reality: if a supplement isn’t absorbed well, it doesn’t matter how elegant the biochemistry is.
Bioavailability is the fraction of what you take that your body actually absorbs and can use. CoQ10 is fat-soluble, so absorption depends on:
Your body needs both these forms, so either can serve as an input. But formulation, age, digestion, and dose timing can influence real-world absorption. If you want the “forms + function” explanation: The Three Faces of CoQ10
Let’s clear something up before we go further. Despite some marketing claims to the contrary, ubiquinone is not ‘inactive,’ nor is ubiquinol the only biologically useful form. In reality, both forms are biologically active and continuously interconvert in the body, but they tend to operate in different physiological contexts. It’s also worth noting that most of the clinical studies reporting positive cardiovascular effects of CoQ10 - including those in chronic heart failure - used the ubiquinone form, largely because it was the form available when much of the foundational research was conducted. Ubiquinol is more commonly found in peripheral tissues and circulation, where it participates in antioxidant defense, while ubiquinone is more heavily sequestered within mitochondria, where it plays a central role in energy production - making it less visible in blood measurements, but still the predominant form of CoQ10 at the cellular level.
Additionally, formulation and stability studies have shown that ubiquinol is less chemically stable and may oxidize back to ubiquinone in the gastrointestinal environment prior to or during absorption, with some studies reporting substantial conversion under certain conditions. Together, these factors help explain why both forms can ultimately serve as effective inputs, and why formulation quality, dose, and absorption context may matter more than the specific label on the bottle.23
Clinical studies have used doses ranging roughly from 60 to 1,200 mg/day, depending on condition and design.25
A key practical concept is non-linear absorption: at higher single doses, a smaller fraction may be absorbed as there is a limit to how much CoQ10 the gut can absorb at any one time. This is one reason people split larger totals into smaller doses (for example, 100-200 mg servings) to improve tolerability and possibly absorption dynamics.24
For a full dosing logic guide: CoQ10 Dosage Explained: How Much Should You Really Take?
Yes. CoQ10 can interact with medications (including anticoagulants and other medications for chronic disease states), so it’s not something to casually stack on top of prescriptions without talking to a clinician.26
A good conversation isn’t “Should I take CoQ10?” It’s:
If statins are part of your care, you may be interested in our articles on the topic:
CoQ10 is a real molecule doing real work in your cells - especially in mitochondrial energy transfer and antioxidant redox cycling. That makes it biologically relevant to the heart.
Clinically, the evidence in this article’s reference set is strongest for adjunctive support in chronic heart failure, with more mixed/modest evidence for blood pressure, and less direct evidence for outcomes like arrhythmias or atherosclerosis progression (where mechanisms are plausible but clinical certainty is lower).3, 4, 5
The most balanced approach is: use CoQ10 thoughtfully, not magically - as one tool that may help some people, alongside the foundations of cardiovascular health and appropriate medical care.
If, after consulting with your physician or healthcare provider, you decide that supplementing with coenzyme Q10 may be appropriate for you, we offer our premium CoQ10 for your consideration. No specific brand has been shown to produce superior clinical results, but not all supplements are created equal. Regardless of the product you choose, look for a quality supplement that is third-party tested for both potency and purity, is manufactured at a certified facility, and aligns with your individual health needs.
Regulatory Disclaimer:
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
CoQ10 may benefit heart health by supporting energy production in heart cells, acting as a potent antioxidant to combat oxidative stress, and helping to improve blood vessel function, which helps maintain cardiovascular health.
CoQ10 plays a vital role in energy production by helping generate ATP, the main energy source for heart cells. This is essential for keeping the heart functioning efficiently, given its high energy demands.
Maybe. Although there are studies that have shown CoQ10 to improve symptoms in individuals with heart conditions like heart failure, hypertension, and angina, there is not yet enough evidence to state this unequivocally. Its ability to boost energy production and reduce oxidative stress are mechanisms that explain how CoQ10 may help in managing these conditions.
CoQ10’s ubiquinol form acts as a powerful antioxidant that neutralizes free radicals, which may help protect heart cells from oxidative damage - a major contributor to heart disease.
Possibly. Statin users are often recommended to take CoQ10 supplements because statins reduce the body’s natural CoQ10 production. Supplementing with CoQ10 may help reduce muscle pain and fatigue caused by statins.
Ubiquinone and ubiquinol are both forms of CoQ10. Ubiquinone is the oxidized form and is primarily used for energy production, while ubiquinol is the reduced form, which functions as an antioxidant. Both forms are effective, and the body can convert between them as needed.
The recommended daily dosage for CoQ10 can range from 60 to 1,200 mg, depending on individual health needs and specific heart and health conditions. It’s important to split higher doses throughout the day for better absorption. Check with your doctor to help determine what dose is best for you.
CoQ10 is generally well-tolerated, but some individuals may experience mild side effects such as insomnia, dizziness, or gastrointestinal discomfort. Serious side effects are rare, but it’s always a good idea to consult with a healthcare provider before starting supplementation.
Individuals with conditions affecting their heart health, those on statin medications, and those seeking to enhance energy levels, improve fertility, reduce fatigue and muscle weakness, and improve mental acuity are more likely to benefit from CoQ10 supplementation.
1: Cleveland Clinic. How the Heart Works. Retrieved from [Cleveland Clinic
2: Gertz EW, Wisneski JA, Neese R, Bristow JD, Searle GL, Hanlon JT. Myocardial lactate metabolism: evidence of lactate release during net chemical extraction in man. Circulation. 1981;63(6):1273-1279.
3: Crane, F.L., 2001. Biochemical functions of coenzyme Q10. Journal of the American College of Nutrition, 20(6), pp.591-598.
4: Folkers K, Langsjoen P, Willis R, et al. Lovastatin decreases coenzyme Q levels in humans. Proc Natl Acad Sci U S A 1990;87:8931-4.
5: Littarru GP, Tiano L. Bioenergetic and antioxidant properties of coenzyme Q10: recent developments. Mol Biotechnol 2007;37:31-7.
6: Eckers A, Haendeler J. Endothelial cells in health and disease. Antioxid Redox Signal. 2015 May 10;22(14):1209-11. doi: 10.1089/ars.2015.6323. PMID: 25758789.
7: Belardinelli, R., Muçaj, A., Lacalaprice, F., Solenghi, M., Principi, F., Tiano, L., Littarru, G.P. and Tavazzi, L., 2005. Coenzyme Q10 improves contractility of dysfunctional myocardium in chronic heart failure. Biofactors, 25(1‐4), pp.137-145.
8: Mortensen, S.A. et al., 2014. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure. JACC: Heart Failure, 2(6), pp.641-649.
9: Rosenfeldt, F. et al., 2007. Coenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials. Journal of Human Hypertension, 21(4), pp.297-306.
10: Aydin, A. et al., 2000. Short-term oral coenzyme Q10 treatment in patients with high level of lipoprotein(a). Journal of Clinical Biochemistry and Nutrition, 29(2), pp.81-89.
11: Langsjoen, P.H. and Langsjoen, A.M., 2007. The clinical use of HMG CoA-reductase inhibitors and the associated depletion of coenzyme Q10. A review of animal and human publications. Biofactors, 18(1-4), pp.101-111.
12: Belardinelli, R., et al., 2006. Coenzyme Q10 and exercise training in chronic heart failure. European heart journal, 27(22), pp.2675-2681.
13: Hidaka, T., et al., 2008. Safety assessment of coenzyme Q10 (CoQ10). Biofactors, 32(1-4), pp.199-208.
14: Soja, A.M., and Mortensen, S.A., 1997. Treatment of congestive heart failure with coenzyme Q10 illuminated by meta-analyses of clinical trials. Molecular Aspects of Medicine, 18, pp.159-168.
15: PDQ Integrative, Alternative, and Complementary Therapies Editorial Board. PDQ Cancer Information Summaries [Internet]. National Cancer Institute (US); Bethesda (MD): Jun 7, 2022. Coenzyme Q10 (PDQ®): Health Professional Version.
16: Drugs and Lactation Database (LactMed®) [Internet]. National Institute of Child Health and Human Development; Bethesda (MD): May 17, 2021. Coenzyme Q10.
17: Baggio E, Gandini R, Plancher AC, Passeri M, Carmosino G. Italian multicenter study on the safety and efficacy of coenzyme Q10 as adjunctive therapy in heart failure. CoQ10 Drug Surveillance Investigators. Mol Aspects Med. 1994;15 Suppl:s287-94.
18: Feigin A, Kieburtz K, Como P, Hickey C, Claude K, Abwender D, Zimmerman C, Steinberg K, Shoulson I. Assessment of coenzyme Q10 tolerability in Huntington's disease. Mov Disord. 1996 May;11(3):321-3.
19: Saini, R., 2011. Coenzyme Q10: The essential nutrient. Journal of Pharmacy & Bioallied Sciences, 3(3), p.466.
20: American Heart Association. 2020. The American Heart Association Diet and Lifestyle Recommendations.
21: Steptoe, A., Kivimäki, M. 2012. Stress and cardiovascular disease. Nature Reviews Cardiology, 9(6), pp.360-370.
22: Mayo Clinic. 2021. Heart disease: Prevention.
23: Judy, W. V., Stogsdill, W. W., & Judy, D. S. 2007. Coenzyme Q10: Facts or Fabrications? Natural Products Insider.
24: Mayo Clinic. 2021. Coenzyme Q10.
25: Weis M, Mortensen SA, Rassing MR et al. Bioavailability of four oral coenzyme Q10 formulations in healthy volunteers. Mol Aspects Med 1994;15:273–80.
26: National Institutes of Health. 2021. Coenzyme Q10: In Depth.
Although I am a doctor, I am not your doctor. Before making any changes to your current treatment regimen—including adding CoQ10—discuss your options with a healthcare provider who knows you, your history, and your health goals.
Whether you are much interested in investing, our collection of articles is designed to educate and empower you.